E 8 Radiant Warmer
This equipment is mainly important for Hypothermia as decribed in
Prevention and Management of Hypothermia.
Subsection of this chapter:
- Clinical Problem
- Assessment
- Management
- Infection Prevention
- Complications
- Care & Maintenance
- Troubleshooting & Repair
NEST360°. Newborn Essential Solutions and Technologies-Education – Clinical Modules: Radiant Warmer. (June 2020). License: CC BY-NC-SA 4.0.
Clinical Problem
Temperature less than 36°C at birth has been recognised as an independent risk factor for death in preterm infants. 1,2
Radiant warmers may be used on any neonatal patient admitted to the nursery ward, but
especially for:
OBSTETRIC & LABOUR NOTE
In stable newborns priority should always be given to skin-to-skin and KMC over
artificial warming devices. Unstable babies and any requiring resuscitation need an
area post-delivery to prevent hypothermia. Using pre-warmed towels, neonatal patients
should immediately be dried, with one towel that is then discarded and replaced by
another dry one, wrapped and placed under a radiant warmer following delivery. Newborn
babies can drop their body temperature very quickly, even within minutes. They must be
kept warm from the moment of birth, during their time in the labour ward and when
transferred to the nursery. Even small drops in temperature increase the likelihood
of mortality.2–4
Extremely premature babies can be placed in a clean plastic bag immediately after birth,
without prior drying and ensuring the head is kept free from the plastic.4
(1.1) The head
is covered with a hat. This assists prevention of heat loss. A baby in a plastic bag must
be monitored very frequently to prevent overheating.

Regardless of location, it is preferential to start patients on
Kangaroo Mother Care if it is
clinically appropriate and the patient is stable.
Assessment
However warm a room may feel to an adult, a neonate can lose heat. This heat loss
in neonatal patients is rapid, with hypothermia directly contributing to mortality.2–4
Radiant warmers (2.1) use overhead heating elements to provide radiating heat
ensuring maintenance of normothermia.
Newborn babies lose heat through four main mechanisms.5
- Evaporation: water loss through the skin.
- Radiation: heat radiating from the warmer patient towards cooler surfaces (e.g., windows
or walls).
- Conduction: direct heat travel from warmer surface of the skin to the cooler mat or cot on
which the patient rests.
- Convection: air currents move heat away from the skin/body.
Radiant warmers provide radiating heat to minimise metabolic requirements for heat
production, decreasing the risks of hypoglycaemia and respiratory distress associated
with hypothermia. Radiant warmers provide an area where resuscitations, procedures,
and short-term observation can take place while keeping the baby warm. Warmers may
vary in complexity, including only heating functionality or heating functionality with
resuscitation and oxygen equipment. All warmers include a temperature probe that
provides information on the patient’s temperature. (2.2)


Radiant warmers heat in various modes, the names of which may vary based on device:
(2.3)
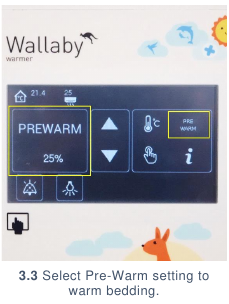
- Prewarm: provides constant low heat for a short amount of time (typically 10 minutes or
less) to prepare the cot underneath the warmer to receive a patient.
- Automatic: also called servo or baby mode; uses a temperature probe on the baby to
automatically adjust heat provided to maintain the patient’s temperature within an
acceptable range.
- Manual: provides a constant, unadjusting heat that is set by the user. Patients should
never be left unattended if being treated in manual mode.

Normothermic axillary temperature in neonates ranges from 36.5oC to
37.5oC.4,5 Every effort
must be made to keep a baby's temperature within the normal range as temperature below
36oC is an independent risk factor for death in newborns.1,2
Management
Management covers how to use the radiant warmer, including set up for a patient,
patient preparation & commencement, care whilst on the device & removal of the
patient from the device
SETTING UP FOR A PATIENT
- Plug power cable into the radiant warmer. (3.1) Plug power cable into a wall socket
& surge protector if available and switch on the power. (3.2)


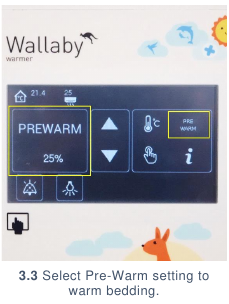
- Select manual setting at 25% or Prewarm setting (if available on model). (3.3)
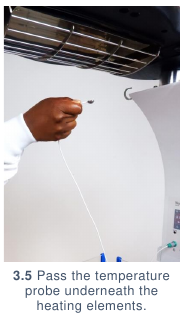
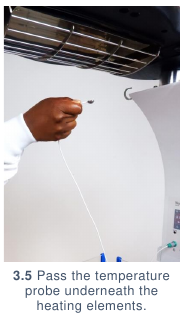
- Plug temperature probe into the infant temperature probe port. (3.4) Hold
temperature probe in hand and move hand directly under overhead heating
elements to check for heat. (3.5) You should be able to feel heat emitting from the
heating elements. (3.6) Allow bedding to grow warm while waiting for the baby to
arrive in the nursery, be transferred to the radiant warmer, or be delivered in the
labour ward.


PREPARING A PATIENT
- Collect:
- Always explain the purpose, risks, and benefits of a procedure to guardians BEFORE
performing the procedure.
- Follow handwashing protocol.
- Ensure patient is dry from any birth fluids or bodily secretions and is wearing a hat to
prevent excess heat loss from the head.
STARTING A PATIENT
- Ensure radiant heater has been prewarmed. If the radiant warmer has not been
prewarmed, then take steps to do so. Prewarming is essential in order to prevent infant
from losing heat to the mattress when initially placed on the warmer.
- Change the radiant warmer from Pre-Warm to select Servo/Automatic mode. (3.7)
- Position infant in middle of radiant warmer cot, maintaining additional treatment tubing
(e.g., CPAP tubing, IV lines) in place. (3.8)


- Use gauze and 70% alcohol to clean temperature probe.
- Place temperature probe directly above infant’s liver and secure with tape or elastic
bandage. (3.9) If a child with myelomeningocele needs to be cared for prone, then place
the probe over the infant’s flank. The probe should be secured firmly enough that it will
not fall off the patient, but not so firmly that it is pressing into the infant’s skin.

- If used in servo mode, the goal temperature for the baby is usually set to a default 36.50C.
The user may change the goal temperature depending on patient’s clinical status.
- Ideally, each radiant warmer should be used for one baby with a temperature probe
dedicated for that patient. Sharing of a radiant warmer and temperature probe poses a
risk for temperature regulation and infection control. If multiple patients are sharing one
warmer, regular temperature monitoring must be conducted using a temperature probe or
thermometer. If the radiant heater is used in manual mode, the baby must be constantly
attended as there is a real danger of overheating.
CARING FOR A PATIENT
- Monitor the patient’s temperature 5 minutes after starting on radiant warmer, and then 4
hourly (if in servo mode) or every 30 minutes (if in manual mode).
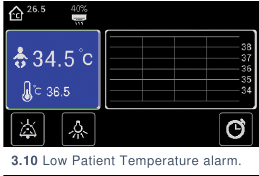
- Pay close attention to any alarms:
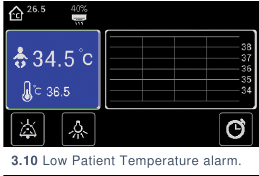
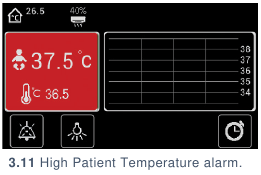
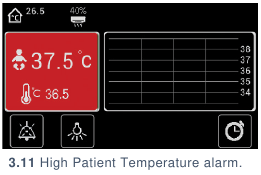
- Temperature: the infant temperature probe has recorded temperatures below
(3.10) or above (3.11) the safe range for the patient. Assess if the patient is too hot
or cold and change the radiant warmer settings accordingly. Check probe is not
dislodged from the baby.
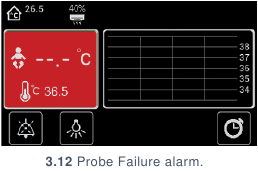
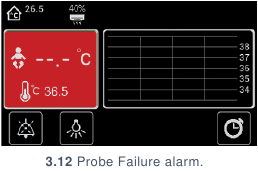
- Probe: the temperature probe is not secured in the radiant warmer appropriately
or the probe has malfunctioned. (3.12) Make sure the probe is plugged in; if the
alarm continues, replace the probe or contact your maintenance department.
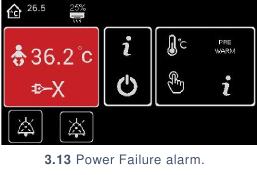
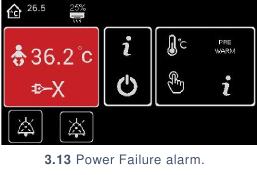
- Power: the mains power has failed. (3.13) Turn off the power button on the radiant
warmer control and move the patient to a working warmer.
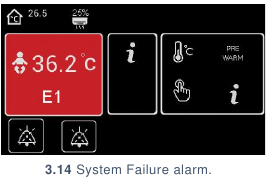
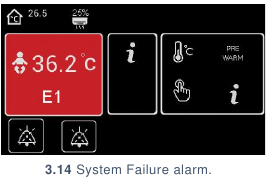
- System: the radiant warmer has recorded a problem with its system. (3.14) This
may result in the radiant warmer no longer providing heat or no longer monitoring
the patient. Move the patient to a working warmer and contact your maintenance
department.
REMOVING A PATIENT
- Collect:
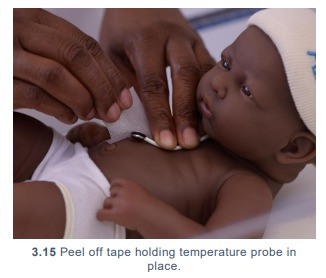
- Gently remove tape/bandage holding temperature probe from patient. (3.15)
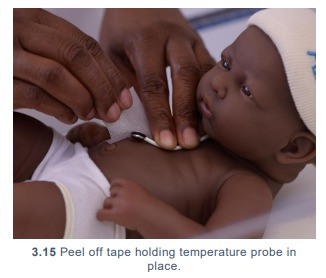
- Disinfect probe site on patient and temperature probe with gauze and 70% alcohol.
- Turn off warmer using switch and unplug.
- Check the patient’s temperature after 30 minutes off the warmer, to ensure normal
body temperature is maintained.
- Disinfect the cot before reuse.
Infection Prevention
Routine and adequate cleaning of medical devices is critical to prevent hospital-acquired infections in newborn care units.
GENERAL INFECTION PREVENTION
- Clean hands with soap and water or 70% alcohol before and after placing a patient
in a radiant warmer or handling any consumables that will be used on a patient
(e.g., temperature probe).
- Ensure that all patient-related consumables (including probes) are new or have
been cleaned thoroughly before use. Any patient-related consumables must be
cleaned before they are used to assess another patient on the radiant warmer.
- All patient-related consumables should be stored in a clean, dry location. Any
cables should be loosely wrapped and secured, preventing sharp bends or kinks,
which will decrease the lifetime of the cables. Do not pinch or bend the cables.
- As mentioned in Radiant Warmer: Management, each radiant warmer should be
used for one baby with a temperature probe dedicated for that patient. Sharing of
a radiant warmer and temperature probe poses a high risk for infection
transmission between patients. If the patient probe and surfaces are not cleaned
thoroughly before use, infection can also be transmitted.
DISINFECTION AFTER USE
- Turn off and unplug the radiant warmer, if not using with another patient. Allow to
cool.
- After every use, use gauze and 70% alcohol or diluted chlorine (Alert 4.1) to
thoroughly wipe:
- Temperature probe, including cable and plug head
- Control panel
- Power button
- Mattress – cleaning both sides
- Cot walls
- Housing of the radiant warmer should be cleaned according to ward guidelines for
disinfecting surfaces.
| ! |
ALERT 4.1 |
| Disinfection of equipment should always comply with manufacturer
guidelines. General guidance on environmental cleaning and disinfection
of equipment was taken from the Infection Prevention and Control:
Reference Manual for Health Care Facilities with Limited Resources,
Jhpiego, Module 66 which lists isopropyl alcohol (70-90%), sodium
hypochlorite (0.05% or >100ppm available chlorine) quaternary
ammonium, and Iodophor germicidal detergent as appropriate for low level
disinfection. Phenolic germicidal detergent is also listed in this category but
should not be used in neonatal wards since affordable, effective
alternatives are available; and, there are concerns it may cause
hyperbilirubinemia and/or neurotoxicity in neonates.7
When utilising re-processed devices meant for single-use (like temperature
probes), careful attention must always be paid to assure that devices are
continuing to function properly.
|
Complications
Introduction of equipment in newborn care units poses clinical and device
Ethics application 3463complications for patients. Awareness of potential
complications is critical to maximise patient safety.
CLINICAL COMPLICATIONS
- Hypothermia & cold stress: if the device is not prepared correctly, is malfunctioning, or
the baby is left exposed for a long period of time, there is a risk of hypothermia. This is
associated with a significant increase in mortality and morbidity including respiratory
distress syndrome, metabolic derangements, interventricular haemorrhage, and late onset
sepsis.4 Hypothermia additionally increases the risk of necrotising enterocolitis in preterm
infants.2,4 If a baby is cold, rewarming must be careful and gradual.
- Hyperthermia & heat stress: hyperthermia can occur in patients whilst on manual mode
who are not monitored regularly or on servo mode if the temperature probe falls off as they
may become overheated. Risks of hyperthermia include increased fluid loss with
development of hypernatraemic dehydration, convulsions, increased metabolism,
tachypnoea, tachycardia, and recurrent apnoea.8–12 (Alert 5.1)
- Pressure sores: pressure sores may develop if the patient is incorrectly positioned, is
lying on additional tubing/equipment, or the temperature probe is not positioned correctly.
- Falls: the cot sides of the radiant warmer must be in place to prevent the baby falling off
the mattress on to the floor.
- Infection: if the temperature probe or infant warmer are not cleaned thoroughly before
use, infection can be transmitted. Care should be taken particularly for consumables that
are marked as single-use but are reused in practice (such as temperature probes).
| ? |
ALERT 5.1 Contextualising Hyperthermia
|
There are two ways that an infant might have an elevated core
temperature: (1) infection (2) environmental.
- Infection: In the case that an elevated temperature is generated
by infection, there is no temperature which is considered
“dangerous” and would require additional alarms. Fever, regulated
by the hypothalamus, is the body’s normal response to infection or
inflammation which is induced by cytokine activation.
- Environmental overheating:
- Device overheating: A device overheating an infant can lead
to a number of potentially dangerous outcomes that may
result in serious harm. Environmental overheating is not a
body’s normal response to an illness (as seen in fever) but
rather a mismatch between environmental heat and the ability
of the infant’s body to dissipate heat. Environmental
overheating may result in serious heat related illness
including damage to the central nervous system.8,9 Compared
to older individuals, babies are at particularly high risk of
environmental overheating since they have higher heat
production (metabolic rates), higher surface area to mass
ratios (i.e., higher absorption of heat from environment), less
ability to dissipate heat and no ability to independently access
fluids.10-12
- Maternal heat transference: Immediately following delivery
hyperthermia can be caused by maternal fever during labour
and delivery as foetal temperature is up to 1°C higher than
maternal temperature.13
Note on special circumstances: CNS injury, in which it is critical to avoid
hyperthermia in the first 72 hours following birth, may affect the newborn’s
temperature. However, CNS damage will typically result in temperature
instability rather than hyperthermia.13
|
DEVICE COMPLICATIONS
- Hyperthermia due to probe mismanagement: if the device is set to automatically adjust
its temperature based on the patient’s temperature (servo mode) and the patient
temperature probe falls off the patient or is not well secured (5.1), the radiant warmer may
overheat in an attempt to compensate for what it observes as a low body temperature.
This puts the patient at risk for a body temperature >40oC and clinical harm

- Alarms: radiant warmers have in-built alarms that should sound if the patient’s
temperature is above or below a set normothermic range. If this range is not appropriately
set, alarms may sound at incorrect situations.
- Fire: if linen is placed on the radiant heater head, heat and dust may build up and pose a
fire hazard. Never store linen on top of the device or close to the heating elements.
Although treatment devices (e.g., phototherapy units, oxygen concentrators) can be used
with a radiant warmer, care should be taken to ensure that the direct line of heat to the
patient from the radiant warmer heating elements is not obstructed.
Care & Maintenance
Users are responsible for basic first-line care and maintenance to ensure
equipment lasts to their potential lifetime.
POWER SOURCE
Radiant warmers are powered with mains/socket power. Radiant warmers are typically
the largest consumers of power in a nursery and should be plugged into their own socket
and surge protector if available. (6.1 & 6.2) Radiant warmers typically draw too much
power to be used with small-scale solar systems. In most cases, the cost (both financially
and energetically) to run radiant warmers during a power cut prevents them from being
used with backup power.

WARD LOCATION
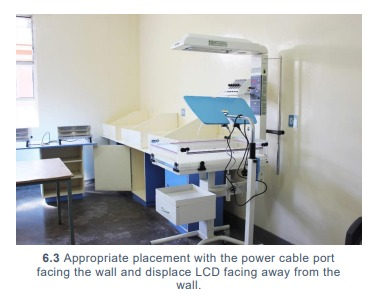
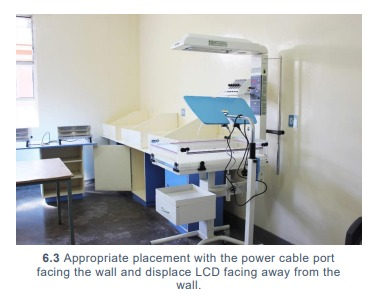
Radiant warmers should be placed against a wall with the power cable/stand facing the
wall and control panel facing the middle of the nursery room. (6.3) Warmers should be
away from any windows to avoid air currents disrupting heat radiation. Windows are
preferably kept closed.
USER PREVENTIVE MAINTENANCE
Preventive maintenance should be conducted weekly and should include:
- Test the heating elements and temperature probe:
- Plug in the machine. Connect the temperature probe. Turn the power switch to
ON. Leave the machine on for 1 minute.
- Hold the temperature probe in the palm of your hand and hold your hand near the
overhead heating elements. Slowly move it from the part of the heating element
closest to the stand, moving towards the outside end of the heating element. You
should feel your hand progressively heat as you move it, and see the temperature
reading on the machine steadily increase.
- If you feel any sections of the heating elements are not providing heat, contact
your maintenance department.
- Test the power loss alarm: while the radiant warmer is plugged in and turned on,
turn off the power at the wall socket. An alarm should sound. If it does not sound,
contact your maintenance department.
Troubleshooting & Repair
Although users are not responsible for repairing their devices, there are steps that
may be taken to troubleshoot first-line errors that may occur before contacting
maintenance or engineering support.
| 1 |
The radiant warmer does not turn on |
|
- Check that the power cable is firmly plugged in to the back of the device. Check
that the power switch on the back of the device is turned on.
- If the power switch is turned on and the power cable is firmly plugged in but the
device is still not turning on, try replacing the power cable.
- Should the radiant warmer still not turn on, contact your maintenance
department.
|
| 2 |
The radiant warmer is turning on, but is not heating
|
|
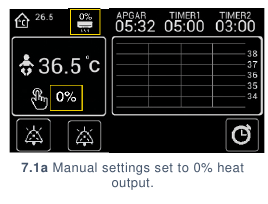
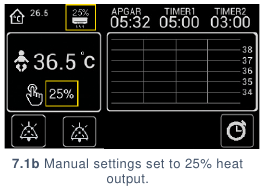
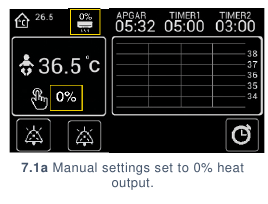
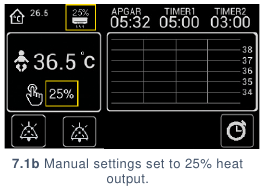
- Check the radiant warmer settings to ensure that heating is turned on: If in
manual, the heating settings may be set to 0%.(7.1a) Make sure that the heater
output is set to a number above 0%.(7.1b)
- If the power switch is turned on and the power cable is firmly plugged in but the
device is still not turning on, try replacing the power cable.
- If the heating settings are turned on & the radiant warmer is still not heating,
contact your maintenance department.
|
| 3 |
The radiant warmer is turning on, but the temperature probe is not reading
the patient’s temperature |
|
- Hold the temperature probe in the palm of the hand and watch temperature
reading on control panel to see if the temperature changes to a reasonable body
temperature.
- If the temperature does not change or there is a “Probe alarm” displayed,
replace the probe with a spare or contact your maintenance department.
|
References
- Mullany, L. C. et al. Hypothermia and associated risk factors among newborns of southern Nepal.
BMC Pediatrics 8, 13 (2010).
- Laptook, A. R. et al. Admission Temperature and Associated Mortality and Morbidity among
Moderately and Extremely Preterm Infants. The Journal of Pediatrics 192, 53-59.e2 (2018).
- Miller, S. S., Lee, H. C. & Gould, J. B. Hypothermia in very low birth weight infants: distribution, risk
factors and outcomes. Journal of Perinatology 31, S49–S56 (2011).
- Perlman, J. M. et al. Part 7: Neonatal Resuscitation: 2015 International Consensus on
Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment
Recommendations (Reprint). PEDIATRICS 136, S120–S166 (2015).
- Essential elements of obstetric care at first referral level. (World Health Organization, 1991).
- Curless MS, Ruparelia CS, Thompson E, and Trexler PA, eds. 2018. Infection Prevention and
Control: Reference Manual for Health Care Facilities with Limited Resources. Jhpiego: Baltimore,
MD.
- Sharma, G. Infection Prevention and Control at Neonatal Intensive Care Units. 134.
- Bouchama, A. & Knochel, J. P. Heat stroke. N. Engl. J. Med. 346, 1978–1988 (2002).
- Bynum, G. D. et al. Induced hyperthermia in sedated humans and the concept of critical thermal
maximum. Am. J. Physiol. 235, R228-236 (1978).
- Bytomski, J. R. & Squire, D. L. Heat illness in children. Curr Sports Med Rep 2, 320–324 (2003).
- Naughton, G. A. & Carlson, J. S. Reducing the risk of heat-related decrements to physical activity
in young people. J Sci Med Sport 11, 58–65 (2008).
- Falk, B. Effects of thermal stress during rest and exercise in the paediatric population. Sports Med
25, 221–240 (1998).
- Ringer, S. A. Core Concepts: Thermoregulation in the Newborn, Part II: Prevention of Aberrant
Body Temperature. NeoReviews 14, e221 (2013).